High blood sugar doesn’t usually feel good and can be alarming if it’s way above your target range. If you’re wondering how to get it down and lower it quickly, I’ve got some tips.
If you ever check your blood sugar, you’ve probably noticed that your numbers are different every time. Even if you check within minutes. Our blood sugars are always changing. Blood sugar fluctuations are normal in EVERYONE. But there may come a time when your blood sugars are above normal. Maybe you’ve been told by your doctor that your blood sugar levels are too high. Let’s do something about it.
In this post, I’ll be using the terms blood sugar and blood glucose. They mean the same thing. Glucose=sugar. Another term for high blood sugar is hyperglycemia. If you have prediabetes or diabetes (type 1, type 2, or gestational), you’ll want to watch out for high blood sugar.

If you’re new here, welcome! I’m Erin, a dietitian and diabetes educator that believes you can achieve your health goals WITHOUT restriction and dieting. Just because you are wanting lower your blood sugar DOES NOT mean you have to starve yourself or go without carbs.
While avoiding carbs is a method people use to lower blood sugar and lose weight, it is not sustainable. I want to provide you with options that are realistic and doable.
What is high blood sugar?
Let’s talk about what is considered a high blood sugar. Normal fasting blood sugar, or before you’ve eaten anything, is under 100 mg/dL. If you have been diagnosed with diabetes, your fasting levels may be a bit higher.
According to the American Diabetes Association, your blood sugar levels should be between 80-130 mg/dL when you are fasting, and less than 180 mg/dL 1-2 hours after a meal. So if your blood sugar is above 180 mg/dL, it is high.
What are the symptoms of high blood sugar?
Most of the time you can feel when your blood sugar is too high, but everyone is different. Common symptoms of high blood sugar include:
- Excessive thirst, like you can’t drink enough water to quench it
- Frequent urination, often up several times during the night to go to the bathroom
- Feeling really tired and low in energy
- Headache
- Blurred vision
Some of these symptoms you may live with for a long time. It often becomes a person’s “normal” and they may not attribute the symptoms to their glucose levels. You can’t always rely on symptoms to know if you have hyperglycemia. The only way to know for sure is to check your blood sugar with a monitor or CGM.
What causes high blood sugar?
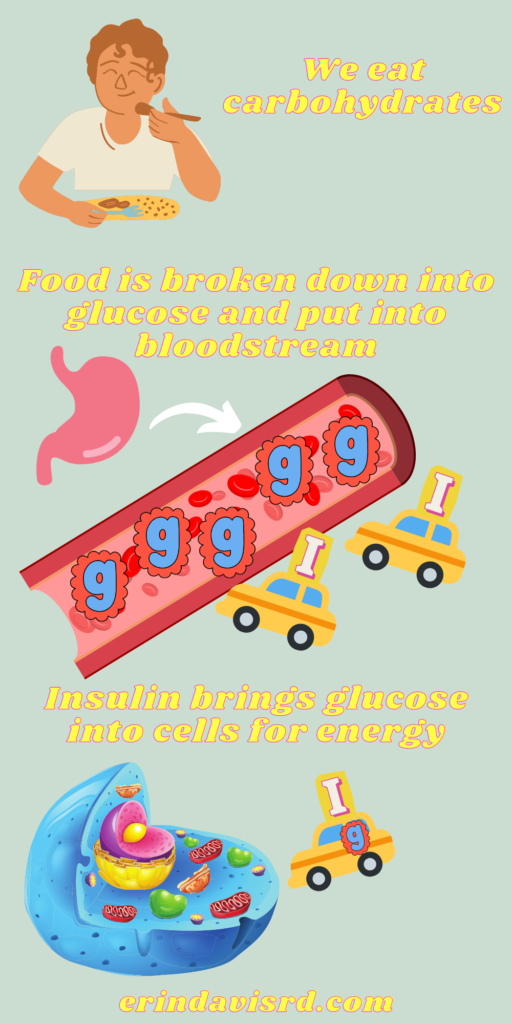
There are a variety of reasons your blood sugar might be high. Of course, what you eat makes a difference in your blood sugar. When we eat something with carbohydrates, our body breaks it down into glucose and releases it into the blood for fuel.
We need that fuel for our brains and body. Our body responds to that glucose in our blood by secreting insulin. Insulin helps get that glucose into the cells where it is needed. Insulin is like a taxi cab and glucose is the passenger. But if you have prediabetes or diabetes, you may not make enough insulin, or your body doesn’t use it well (insulin resistance). That means glucose gets stuck in the blood.
If you’ve eaten more than usual, or have had a meal or snack that was high in simple carbohydrates, you may end up with a high blood sugar. But that isn’t the only thing that makes your blood sugar high. Here are things that may cause hyperglycemia:
- Inactivity
- Sickness or infection
- Stress
- Forgetting to take medication, or not taking enough
- Diet changes-eating larger meals, more carbohydrates
- Hormonal changes
- Poor sleep
What happens when your blood sugar stays high
When you have hyperglycemia, it’s likely that your body is not getting the fuel it needs. So over time, you’ll have zero energy and little focus for even small tasks. But that excess glucose that remains in the blood changes the shape and function of the tiny blood vessels—affecting the nerves, eyes, kidneys, and heart.
Having one or two high blood sugars will likely not do any long-term damage. The problems come when your blood sugar stays elevated for a longer period of time. Some of the major complications from hyperglycemia include nerve damage (neuropathy, or pain and numbness in your feet, legs, and hands), vision impairment, kidney disease, heart disease, and slowed gut function.
How to get your blood sugar down fast
First, I need you to take a deep breath. No need to panic. You’ll get your blood sugar down. Here are some strategies to lower your blood sugar:
- Take rapid or short-acting insulin. Insulin is by far the fastest way to get your blood sugar down. When you are prescribed insulin, you should have a plan in place to correct hyperglycemia. Call your healthcare provider right away if you don’t have dosing instructions.
- Take a walk or do a 10-15 minute exercise video. It’s amazing what a little movement can do for your blood sugars. Note: if you’ve been instructed to check your ketones (type 1) if your glucose is above 240 mg/dL, do so before you exercise. You don’t want to exercise with high ketones.)
- Drink water. Water helps to dilute the excess sugar in your blood. And you’ll replace some of the fluids you’ve lost through those frequent trips to the bathroom.
- Choose lower-carb alternatives. There is no food you can eat to lower your blood glucose. This is one case where I recommend limiting your carbs—temporarily. You are going to honor your body by getting your blood sugar back into the normal glucose range. You may want to stick with protein and veggies when you are wanting to get your blood sugar down fast. If you normally use sugar in your coffee, try a natural sugar alternative, like stevia or monk fruit.




How to lower blood sugar long term
Maybe your glucose levels are just a little elevated. Or perhaps you are dealing with frequent episodes of hyperglycemia. This isn’t something that gets fixed overnight. The target ranges for glucose are set to reduce the risk of complications. Here are some things you can do to reach your blood sugar goals and best manage or prevent diabetes:
- Talk to your healthcare provider: Make sure you are bringing up your concerns with your provider. You want to find a provider that can answer your questions and takes the time to explain things. This is your health and you are in the driver’s seat.
- Enlist the help of a dietitian or diabetes educator: An RD or CDCES (certified diabetes care and education specialist) can help you make the necessary changes in your diet and lifestyle to achieve your health goals. Health education is not a cookie-cutter approach. Diabetes and diabetes prevention education includes many facets and can help address your unique situation.
- Make a physical activity plan: Can you come up with a way to be physically active on a regular basis? It’s recommended you get 150 minutes of physical activity per week. What are your barriers? Movement is essential to making your body more effective at lowering glucose. It doesn’t have to be running on the treadmill. It can be gardening, hiking, tennis, biking, tag with the kids, and more.
- Get adequate sleep: Are you shorting yourself on sleep? Staying up too late while binge-watching your favorite show? It will have an impact on your blood sugars. When we have too little sleep, high cortisol levels can make it difficult to lower our glucose. Aim for 7-9 hours per night.
- Manage your stress levels: Stress, like lack of sleep, can lead to high cortisol levels. Cortisol is a stress hormone that is designed to aid us in survival situations. So while you may need a load of glucose in your bloodstream to run from a charging bear, YOU DON’T need that heightened response to answer emails or perform your everyday tasks. When I work with someone, we talk about sources of stress and healthy coping skills. What’s a way you can lower your stress today?
- Eat consistently: WIth a non-diet approach, we focus on consistency, timing, and quality of food. There are no forbidden foods. So if you want the brownie, eat the brownie. Not some gross, sugar-free, rubbery alternative, but the real thing. Eat it mindfully, with no distractions. Plan for meals and snacks. Don’t go too long between meals in order to prevent extreme hunger and subsequent overeating.
- Take medications as directed: I understand, I’m not the best at following instructions. But those directions on the labels are there for a reason. If you are supposed to take your meds BEFORE your meal, do your best to do just that. Timing is important with blood glucose-lowering medications. And skipping days or weeks will have an impact on your blood sugars. If there is a reason you are unable to regularly take your meds, talk with your provider or CDCES.
- Establish a support system: Chat with friends or family that have similar goals. If you don’t have anyone in your circle that understands, look online for support groups.
- Monitor your blood sugars: The only way to know if your blood sugars are too high is to check them. Do you need help with your monitor? I can help! If you’re sick of poking yourself, talk to your provider about a continuous glucose monitor (CGM). Need a log sheet? Here is one you can download.

It can be stressful and scary to deal with high blood sugar. Remember that you aren’t alone. This stuff doesn’t always come naturally. When you work with me, we’ll pinpoint WHY you are having high blood sugar. Then we’ll come up with a customized plan, just for YOU. Book a free discovery call to see if my services align with your health goals.
About the author
Erin is a registered dietitian and diabetes educator with almost 20 years of experience. She specializes in weight-inclusive diabetes care and prevention, intuitive eating, fitness, and women’s health. She works as a consultant and writer in the health and wellness space. Erin is passionate about empowering people to manage their own health and to have peace with food.


