Diet, exercise, medications, reduce complications. Those are the main things that come to mind when considering diabetes. Eating disorders may not be on your healthcare provider’s radar. However, the coexistence of eating disorders and diabetes happens.
Eating disorders are on the rise. Interestingly, as we learn more about nutrition and increase our public health efforts at fighting against the “obesity crisis”, we’re struggling with more disordered eating behaviors.

Blanket statements are commonly given to people with diabetes. Things like, “Just stop eating carbs”, or “You need to lose X pounds”, with very little guidance beyond that.
Add in the weight bias that so many feel when they are seeking medical care, and it’s easy for eating disorder diagnoses to go untreated.
If you’re new here, welcome! I’m Erin, a registered dietitian and diabetes care and education specialist. I’ve blended my years of experience with diabetes and intuitive eating to provide a non-diet approach for those who have diabetes and other chronic conditions.
I’m very passionate about helping those with disordered eating and diabetes. I want you to know that you are not alone if you struggle with disordered eating while managing a metabolic disorder.
Individuals with diabetes face unique challenges. In some cases, there is a need for meticulous attention to food intake.
Unfortunately, that attentiveness to food often collides with the psychological aspects of an eating disorder.
As a result, the intersection of eating disorders and diabetes is complex. Extreme care needs to be taken when balancing both physical and mental health.
Today’s post is about eating disorders and diabetes. I hope to shed light on the challenges, risk factors, and potential complications. I’ll also provide strategies for support.
Understanding eating disorders and diabetes
From the beginning of your diabetes journey, you are told to monitor numbers. Check your blood sugars, count your carbs, dose your insulin, lose some weight, etc.
While some people with diabetes can manage those numbers without any impact on mental health, I want you to know that it is normal to have a strained relationship with all aspects of those metrics.
For instance, you may have anxiety leading up to a follow-up appointment because you know your A1c will be high. Or you feel like a failure because you’ve not lost the weight your physician recommended you drop.
Has your meter grown dusty because you’ve stopped checking? You know it’ll just be high.
Managing a chronic disease isn’t easy, and can take its toll on your mental health. We know that people with diabetes are more likely to have depression.
All of these pressures can make you dissatisfied with your body, or obsessed with food. Research shows that diabetes may put a person at risk for developing an eating disorder.
Sometimes a good-natured recommendation to restrict your diet to control your diabetes actually screws up your relationship with food.
Types of Eating Disorders
Eating disorders are serious conditions classified as mental health disorders distinguished by rigid and severe eating habits.
Unfortunately, eating disorders can have very serious consequences. With a preoccupation with food and body, an eating disorder can consume a person’s mind and change their personality.
Some of the common eating disorders include:
Anorexia Nervosa

Anorexia is characterized by extreme calorie restriction, intense fear of gaining weight, and distorted body image.
People with anorexia severely restrict food, often meticulously controlling the type and amount of food they eat. There may be rituals assigned to eating, such as breaking a cracker into 10 pieces and eating one piece every hour.
While folks with anorexia may have a skeletal appearance, they believe they are overweight. Their perception of themselves is distorted.
This does not mean that someone who is overweight cannot be diagnosed with anorexia. This is considered atypical anorexia.
There may also be compulsive exercise with a focus on calorie burn. Along with those behaviors, there is an obsession with thinness.
It’s not uncommon for people with anorexia to fixate on food and “thinspo”(images and videos of others likely suffering from anorexia).
There is also a mood component to anorexia. Often those dealing with the condition can be withdrawn, irritable, anxious, and depressed.
Bulimia Nervosa

Bulimia typically involves cycles of binge eating followed by purging behaviors such as vomiting, laxatives, diuretics, enemas, excessive exercise, or fasting.
This isn’t an occasional case of overeating and eating a bit less the next day. Bulimia is characterized by repeated episodes of overeating, often with a loss of control. Essentially, you feel like you can’t stop eating, even though you’re full.
The hallmark of bulimia is that you compensate for the overeating by purging. Purging is mostly done in hiding, as there are feelings of shame and guilt.
One of the more common methods of purging is self-induced vomiting. For example, a person may make themselves vomit after a meal.
Other forms of purging include medications and over-the-counter laxatives, diuretics, and enemas. There may also be extreme exercise routines in place to “undo” the calorie intake.
Binge Eating Disorder

Like bulimia, binge eating includes episodes of consuming large amounts of food, often without control. However, it is without purging behaviors.
According to diagnostic criteria (DSM-5), binge eating episodes are associated with at least 3 of the following:
- Eating faster than normal
- Eating past comfortable fullness
- Eating large amounts of food when not hungry
- Eating alone because of shame and embarrassment
- Feeling disgusted, guilty, and/or depressed
As for how often binge eating occurs, diagnostic criteria state at least 1 day a week for 3 months.
Binge eating disorder, or BED, is the most common eating disorder in people with type 2 diabetes. As you can imagine, binge eating would make it difficult to manage blood sugar.
Additionally, many folks go undiagnosed. Whether it’s fear of judgment, lack of assessment of eating behaviors, or both, many suffer alone.
Diabulimia
A disorder affecting almost 9% of people with type 1 diabetes, diabulimia is characterized by inadequate dosing of insulin with the objective of controlling body weight.
In type 1 diabetes, exogenous insulin (injection or pump) is needed to live. Purposely underdosing or skipping insulin can be very dangerous.
Instead of glucose going into the cells, where it’s needed for energy and primary functions, it is stuck in the blood.
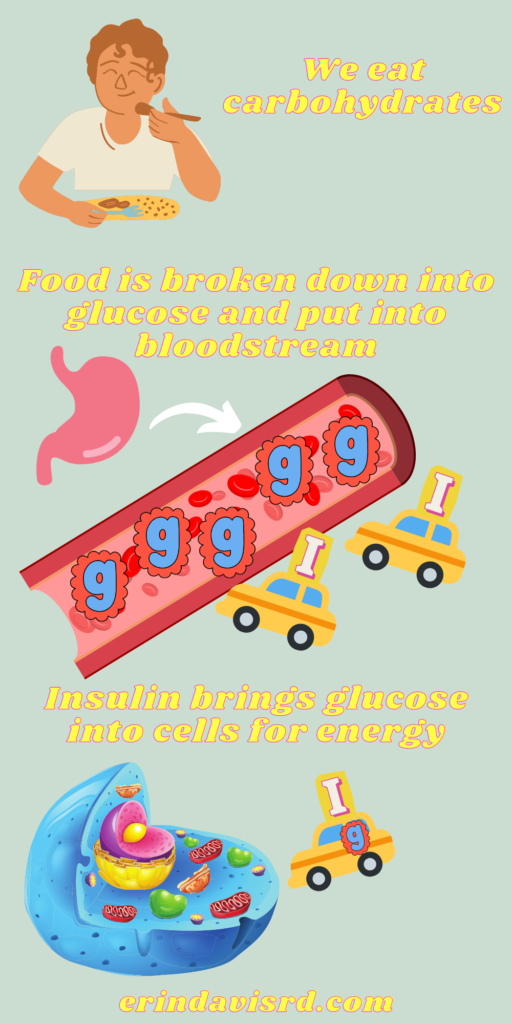
This creates starved cells and a risk for ketoacidosis when the body relies on fat for fuel.
Besides elevated blood sugar, those with diabulima are at risk for fast-tracking short-term and long-term complications associated with diabetes.
Orthorexia

Orthorexia is an obsession with health-related aspects of food. Food choices aren’t necessarily driven by impact on body shape, but rather overall health.
While orthorexia is not considered an official eating disorder diagnosis, it can be debilitating and isolating.
Whether or not orthorexia should be classified as an eating disorder is a debated issue. What matters to me is that it’s a real thing and people with diabetes are at risk.
For example, you stop eating grains, meat, or sugar. You almost fear them because you’ve deemed them unhealthy.
People with orthorexia often will avoid eating out and may talk a lot about food.
How eating disorders complicate diabetes management
Because eating and blood sugar are impossible to separate, it’s obvious that eating disorders will impact your blood sugar in some way.
For individuals with diabetes, maintaining consistent blood sugar levels is crucial. Disordered eating patterns can disrupt this balance, leading to hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar).
Likewise, irregular eating habits, purging behaviors, or extreme dieting can undermine diabetes self-care, potentially leading to long-term complications.
Risk factors for developing eating disorders
There are multiple reasons people develop eating disorders. However, there are some risk factors that make it more likely to occur:
- Genetics
- Gut bacteria/microbiome
- Exposure to disordered eating in youth
- Personality traits (perfectionism, anxiousness)
- Mental health conditions
- Gender
- Socioeconomic status
- Ethnic minority
- Body image issues
- Social influence
- Athlete
- Abuse and trauma
Strategies for support

If you have any disordered eating behaviors, I urge you not to go it alone. You can have freedom from disordered eating.
Here are some ways that you can get help for an eating disorder:
- Integrated Care:
- It takes a village! Eating disorders are complicated and nuanced and will require multiple disciplines for true healing.
- Talk with your primary care provider or endocrinologist about your eating concerns.
- Seek collaborative care involving endocrinologists, dietitians, mental health professionals, and diabetes educators is essential.
- Finding treatment for both diabetes and the eating disorder is crucial for holistic recovery.
- Counseling and Therapy:
- Cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) have shown efficacy in treating both eating disorders and diabetes-related distress.
- Individual and group therapy can provide a supportive environment for addressing psychological and emotional challenges.
- Nutritional Guidance:
- Collaborating with a registered dietitian specializing in both diabetes and eating disorders can help individuals develop a balanced and sustainable approach to food.
Conclusion
Eating disorders and diabetes require a comprehensive and compassionate approach. You should feel understood and heard.
If you’re constantly being pressured by your healthcare team to lose weight or cut carbs, find new providers.
Find yourself a team that will help you work on the physical and mental aspects of these conditions simultaneously.
You can work towards a healthier relationship with food, improved diabetes management, and overall well-being.
It will be a journey, but early intervention, support from healthcare professionals, and a strong support system will help you successfully navigate an eating disorder with diabetes.
If you need help, please reach out. I want you to feel at peace with food and your body. I’m here to listen!
Disclaimer: This information is intended as a self-help tool for your own use, at your own risk. My opinions do not reflect the values, thoughts, or opinions of the Academy of Nutrition and Dietetics or other professional health organizations.
References:
- Dziewa M, Bańka B, Herbet M, Piątkowska-Chmiel I. Eating Disorders and Diabetes: Facing the Dual Challenge. Nutrients. 2023;15(18):3955. Published 2023 Sep 12. doi:10.3390/nu15183955
- Maina JG, Balkhiyarova Z, Nouwen A, et al. Bidirectional Mendelian Randomization and Multiphenotype GWAS Show Causality and Shared Pathophysiology Between Depression and Type 2 Diabetes. Diabetes Care. 2023;46(9):1707-1714. doi:10.2337/dc22-2373
- Berkman ND, Brownley KA, Peat CM, et al. Management and Outcomes of Binge-Eating Disorder [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2015 Dec. (Comparative Effectiveness Reviews, No. 160.) Table 1, DSM-IV and DSM-5 diagnostic criteria for binge-eating disorder. Available from: https://www.ncbi.nlm.nih.gov/books/NBK338301/table/introduction.t1/
- Harris SR, Carrillo M, Fujioka K. Binge-Eating Disorder and Type 2 Diabetes: A Review. Endocr Pract. 2021;27(2):158-164. doi:10.1016/j.eprac.2020.10.005
- Chevinsky JD, Wadden TA, Chao AM. Binge Eating Disorder in Patients with Type 2 Diabetes: Diagnostic and Management Challenges. Diabetes Metab Syndr Obes. 2020;13:1117-1131. Published 2020 Apr 14. doi:10.2147/DMSO.S213379
- Ip EJ, Doroudgar S, Salehi A, Salehi F, Najmi M. Diabulimia: A Risky Trend Among Adults with Type 1 Diabetes Mellitus. Endocr Pract. 2023;29(11):849-854. doi:10.1016/j.eprac.2023.08.001
- Kamarli Altun H, Özyildirim C, Koç Ş, et al. The factors associated with orthorexia nervosa in type 2 diabetes and their effect on diabetes self-management scores. Eat Weight Disord. 2023;28(1):22. Published 2023 Feb 21. doi:10.1007/s40519-023-01552-5
- Barakat, S., McLean, S.A., Bryant, E. et al. Risk factors for eating disorders: findings from a rapid review. J Eat Disord 11, 8 (2023). https://doi.org/10.1186/s40337-022-00717-4
- Bulik CM, Coleman JRI, Hardaway JA, et al. Genetics and neurobiology of eating disorders. Nat Neurosci. 2022;25(5):543-554. doi:10.1038/s41593-022-01071-z
- Navarro-Tapia E, Almeida-Toledano L, Sebastiani G, Serra-Delgado M, García-Algar Ó, Andreu-Fernández V. Effects of Microbiota Imbalance in Anxiety and Eating Disorders: Probiotics as Novel Therapeutic Approaches. Int J Mol Sci. 2021;22(5):2351. Published 2021 Feb 26. doi:10.3390/ijms22052351
- Canals J, Sancho C, Arija MV. Influence of parent’s eating attitudes on eating disorders in school adolescents. Eur Child Adolesc Psychiatry. 2009;18(6):353-359. doi:10.1007/s00787-009-0737-9
- Petisco-Rodríguez C, Sánchez-Sánchez LC, Fernández-García R, Sánchez-Sánchez J, García-Montes JM. Disordered Eating Attitudes, Anxiety, Self-Esteem and Perfectionism in Young Athletes and Non-Athletes. Int J Environ Res Public Health. 2020;17(18):6754. Published 2020 Sep 16. doi:10.3390/ijerph17186754
- Godart N, Radon L, Curt F, et al. Mood disorders in eating disorder patients: Prevalence and chronology of ONSET. J Affect Disord. 2015;185:115-122. doi:10.1016/j.jad.2015.06.039
- Qian J, Wu Y, Liu F, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord. 2022;27(2):415-428. doi:10.1007/s40519-021-01162-z
- Burke NL, Hazzard VM, Schaefer LM, Simone M, O’Flynn JL, Rodgers RF. Socioeconomic status and eating disorder prevalence: at the intersections of gender identity, sexual orientation, and race/ethnicity. Psychol Med. 2023;53(9):4255-4265. doi:10.1017/S0033291722001015
- McLean SA, Paxton SJ. Body Image in the Context of Eating Disorders. Psychiatr Clin North Am. 2019;42(1):145-156. doi:10.1016/j.psc.2018.10.006
- Jiotsa B, Naccache B, Duval M, Rocher B, Grall-Bronnec M. Social Media Use and Body Image Disorders: Association between Frequency of Comparing One’s Own Physical Appearance to That of People Being Followed on Social Media and Body Dissatisfaction and Drive for Thinness. Int J Environ Res Public Health. 2021;18(6):2880. Published 2021 Mar 11. doi:10.3390/ijerph18062880
- Kussman A, Choo HJ. Mental Health and Disordered Eating in Athletes. Clin Sports Med. 2024;43(1):71-91. doi:10.1016/j.csm.2023.07.001
- Caslini M, Bartoli F, Crocamo C, Dakanalis A, Clerici M, Carrà G. Disentangling the Association Between Child Abuse and Eating Disorders: A Systematic Review and Meta-Analysis. Psychosom Med. 2016;78(1):79-90. doi:10.1097/PSY.0000000000000233
- Isomaa R, Backholm K, Birgegård A. Posttraumatic stress disorder in eating disorder patients: The roles of psychological distress and timing of trauma. Psychiatry Res. 2015;230(2):506-510. doi:10.1016/j.psychres.2015.09.044
- Agras WS, Bohon C. Cognitive Behavioral Therapy for the Eating Disorders. Annu Rev Clin Psychol. 2021;17:417-438. doi:10.1146/annurev-clinpsy-081219-110907
- Lammers MW, Vroling MS, Crosby RD, van Strien T. Dialectical behavior therapy compared to cognitive behavior therapy in binge-eating disorder: An effectiveness study with 6-month follow-up. Int J Eat Disord. 2022;55(7):902-913. doi:10.1002/eat.23750
About the author
Erin is a registered dietitian and diabetes educator with almost 20 years of experience. She specializes in weight-inclusive diabetes care and prevention, intuitive eating, fitness, and women’s health. She works as a consultant and writer in the health and wellness space. Erin is passionate about empowering people to manage their own health and to have peace with food.


