Have you recently been diagnosed with gestational diabetes? Wondering what to do next? No need to panic! Today, I’ll be breaking down the basics of gestational diabetes, and sharing what you need to do in order to have a healthy delivery.
It’s a test most women dread. I can’t tell you the number of pregnant clients I’ve had who are nervous before the glucose test.
Usually, at around 24-28 weeks, a pregnant woman will take a 50-gram glucose tolerance test. That is a 1-hour test, where you usually drink a little bottle of “flat pop”.
An elevated result during this test leads to a diagnosis or the 3-hour test. Women often meet with me, discouraged that they “failed” their test.
However, I don’t like to think of it as a failure! It is an elevated result. Failure makes it sound like it is something you did or didn’t do.
All it means is that the test found exactly what it set out to find—your body’s response to a load of glucose, or sugar.
If you’re new here, welcome! I’m Erin, an anti-diet dietitian specializing in diabetes and PCOS. I am passionate about helping women ditch dieting for good, and approach their conditions without restriction.
So what happens when the test detects that your blood sugar remains high after drinking the glucose drink? You are diagnosed with gestational diabetes.
Today’s post is all about gestational diabetes. What it is, how it may impact your baby, and strategies to manage it.
Let’s jump in!
Please note: As an Amazon Associate, I earn from qualifying purchases.
What is gestational diabetes?
Gestational diabetes mellitus, or GDM, is a form of diabetes that develops during the later part of pregnancy.
Hormones are being excreted by the placenta throughout the pregnancy which can cause some insulin resistance. To understand gestational diabetes, I’ll explain how insulin works.
When we eat carbohydrates (bread, pasta, rice, fruit, sweets, etc.), they get broken down into glucose (sugar) molecules. Glucose then gets absorbed into the bloodstream.
Our bodies need to get the glucose from the blood into the cells for energy. It is our fuel. To move the glucose, we need insulin.
Insulin is a hormone excreted by our pancreas that enters our bloodstream to transport glucose into the cell for use.

To simplify things even more, think of a car in need of gas. That car is like our cells. We drive the car to a gas station that has the fuel we need. The gas station is our bloodstream.
But for the gas to get from the gas station to the car, we need the pump with the nozzle. If there are no pumps, all of the fuel is stuck at the station, and all of our cars are on empty!
The pump with the nozzle is insulin. It helps get the fuel in the car.
So, the pregnancy hormones cause the insulin to not work as effectively. The glucose, or fuel, gets stuck in the bloodstream. This means the blood glucose or blood sugar levels get too high.
How does gestational diabetes affect the baby?
Now, what if the blood glucose remains elevated for the remainder of the pregnancy? Well, that baby is being fed by the placenta and the blood supply.
If that blood is high in glucose, the baby’s body will overcompensate by making more insulin.
When the baby is born, it no longer receives that steady supply of blood with elevated glucose levels. Instead, it relies on breastmilk or formula to sustain blood glucose.
However, the baby continues to make extra insulin, and it doesn’t match the amount of glucose in their blood. Therefore, the baby is at risk for having low blood glucose.

Another risk is that as that baby is receiving extra fuel from mom’s blood, they grow bigger than normal. As a result, delivery can be complicated by the size of the baby.
This increases the risk of c-section deliveries. While you can recover from a c-section, it will just take a bit longer for your body to heal.
Gestational diabetes blood glucose targets

What should your blood glucose levels be at during pregnancy? Here are the American Diabetes Association (ADA) recommended blood sugar targets:
- Fasting: 70-95 mg/dL
- 1-hour post-prandial (after eating): 110-140 mg/dL or lower
- 2-hours post-prandial (after eating): 100-120 mg/dL or lower
If you check immediately after eating, it will likely be high. It takes some time for your blood sugars to go down after eating.
10 steps to manage gestational diabetes
Don’t stress! Just because you have been diagnosed with gestational diabetes, doesn’t mean you have to have the complications.
Keeping blood sugars within target will help you avoid the risks associated with gestational diabetes. Here are some actions to take to manage your blood sugar:
1. Coordinate care with your OB-GYN

Most often, an OB-GYN will refer you to a specialist or a diabetes educator to help you manage your blood glucose during pregnancy.
If not, I highly suggest you find someone who will work closely with you for the duration of your pregnancy.
2. Get a glucometer
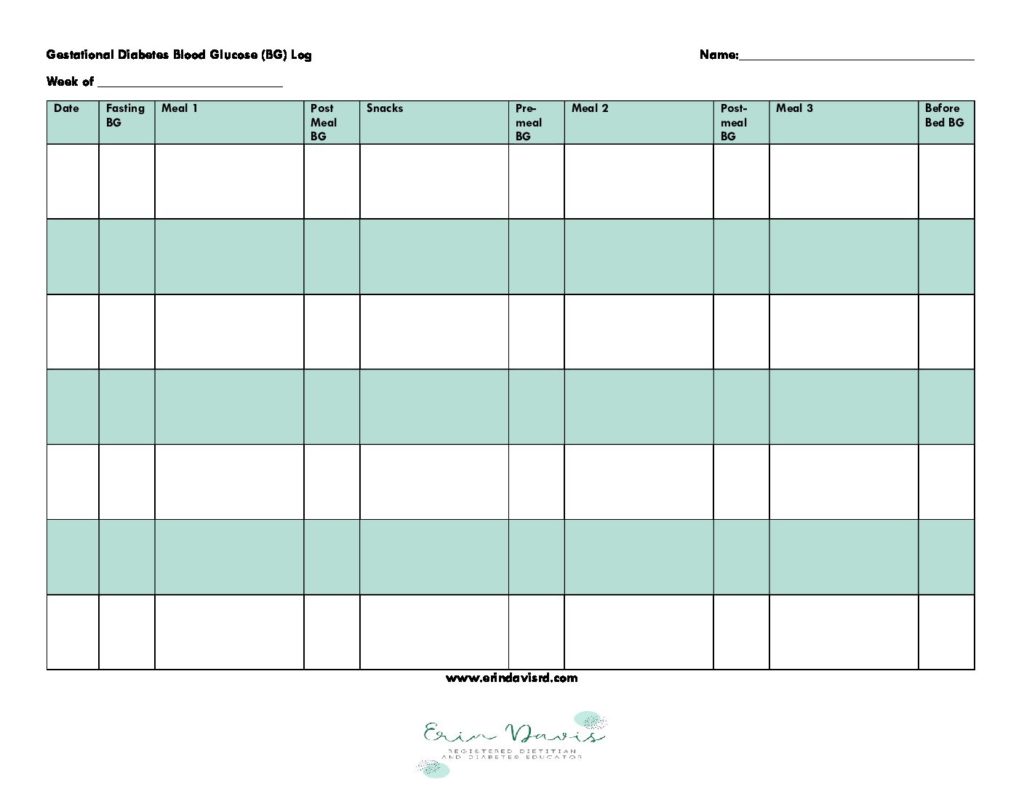
Your OB-GYN and diabetes specialist will want a record of your blood glucose levels. A glucometer, or glucose monitor, will show what your blood glucose levels are doing.
While continuous glucose monitoring (CGM) is occasionally used, the most recent ADA guidelines state there is insufficient data to recommend CGM use for gestational diabetes.
However, I’ve had multiple clients use CGMs during pregnancy with success. The majority use a glucometer, though.
You’ll want to check your blood glucose fasting, and 1-2 hours after a meal. Need a way to track? Get your free blood glucose log printable!
3. Spread out your carbohydrates

Having gestational diabetes does not mean that you can no longer eat carbohydrates. In fact, glucose is required to fuel your pregnancy and the recommendation is around 175 grams of carbohydrates.
Now, I’m not saying you have to carry around a calculator to figure out the number of carbs you are eating. There is a way to simplify it.
Rather than cutting carbohydrates, you can look at what you’re currently eating and make some tweaks to improve glucose levels.
You can eat intuitively with diabetes.
For example, suppose you’re having a mocha latte, a bagel, and fruit for breakfast. All those carbs at once, especially in the morning when you are more likely to struggle with high blood sugars, will make it difficult to come under target.
Instead, you could try a latte with almond milk and stevia sweetener, and an egg sandwich with sauteed veggies on a whole wheat English muffin.
Later in the morning, or at lunch, have your fruit—pairing it with protein and fat.
4. Eat your protein and fat first
There is research that supports the idea of food order. When you save your carbs for last, you may end up with a lower post-meal blood sugar.
And there’s even better results when your carb is high in fiber. So try to swap out your white flour and processed carbs for the more whole-food form (i.e., whole grain pasta, whole wheat bread, brown rice, etc.)
5. Eat mindfully

When we are on-the-go, it is easy to eat with distractions. Therefore, ignoring our fullness signals.
When you eat your meals, do not scroll through your phone or answer emails. Take the time to enjoy your food, and listen to your body. It will tell you when you have had enough.
Here are some mindful eating activities to try to be better in tune with your body’s hunger and fullness cues.
6. Find movement you enjoy

Moving your body will help your body use up some of that extra glucose. It will also help your insulin to work better.
You don’t have to start anything strenuous. Low-impact exercises are great during pregnancy. I also have this post with my favorite workouts for busy moms.
7. Don’t aim for weight gain

Generally, there is a recommended amount of weight gain during pregnancy. Research has found that gaining less than the recommended weight resulted in better outcomes for those with gestational diabetes.
I’m not saying you need to worry about every pound. Rather, don’t purposely increase calories if you’re not feeling hungry.
Recommendations for increased calorie intake and weight gain are external cues for eating. Pay attention to your body’s cues instead.
8. Reduce stress
What is your favorite way to relieve your stress? Perhaps it is spending time with friends and family, devoting time to prayer or meditation, reading a good book, or watching a movie.
Prioritize stress relief and find support. Stress can negatively impact your glucose levels and can make it difficult to make healthy choices.
Too much stress for you to bear? Please get help. One recent study showed that mindfulness-based stress reduction counseling can effectively reduce blood glucose.
9. Get enough sleep

Not only does poor sleep, or sleep disorders, put you at risk for developing gestational diabetes, but lack of sleep will also make it difficult to manage glucose levels.
When you don’t get enough sleep, cortisol levels can increase. Consequently, your morning blood sugar may be too high. And you’ll likely be craving food all day.
It is recommended that you get 7-9 hours of sleep, which I know can be challenging during pregnancy! I wrote this article for DiaTribe, providing sleep tips to optimize blood glucose levels.
10. Take medications as directed

If you need to take insulin during your pregnancy, I want you to know that it isn’t anything you’ve done. There’s no shame. You’re only taking steps to care for your baby.
Insulin is the go-to medication for the treatment of high blood sugar during pregnancy. It doesn’t cross the placenta, so it is completely safe for pregnancy.
It’s important to follow your physician’s or diabetes educator’s instructions on the use of your insulin. Doses may frequently change in response to your blood sugar levels.
You got this!
My hope is that after reading this post, you are equipped to manage those glucose levels for the rest of your pregnancy.
Gestational diabetes doesn’t have to be scary. You can have a healthy pregnancy and delivery! Do you need help with your diet? Having trouble getting your blood sugars to target? I can help.
Book an appointment and I can personalize recommendations to fit your lifestyle and needs.
Disclaimer: This information is intended as a self-help tool for your own use, at your own risk. My opinions do not reflect the values, thoughts, or opinions of the Academy of Nutrition and Dietetics or other professional health organizations.
References
- Sweeting A, Wong J, Murphy HR, Ross GP. A Clinical Update on Gestational Diabetes Mellitus. Endocr Rev. 2022;43(5):763-793. doi:10.1210/endrev/bnac003
- Ye W, Luo C, Huang J, Li C, Liu Z, Liu F. Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. 2022;377:e067946. Published 2022 May 25. doi:10.1136/bmj-2021-067946
- ElSayed NA, Aleppo G, Aroda VR, et al. 15. Management of Diabetes in Pregnancy: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S254-S266. doi:10.2337/dc23-S015
- Mustafa HJ, Seif K, Javinani A, et al. Gestational weight gain below instead of within the guidelines per class of maternal obesity: a systematic review and meta-analysis of obstetrical and neonatal outcomes. Am J Obstet Gynecol MFM. 2022;4(5):100682. doi:10.1016/j.ajogmf.2022.100682
- Kubota S, Liu Y, Iizuka K, Kuwata H, Seino Y, Yabe D. A Review of Recent Findings on Meal Sequence: An Attractive Dietary Approach to Prevention and Management of Type 2 Diabetes. Nutrients. 2020;12(9):2502. Published 2020 Aug 19. doi:10.3390/nu12092502
- Zeinabeh MZ, Atefeh A, Masumeh GHP, Tania D, Mojgan S, Katayoun A. The Effect of Mindfulness-Based Stress Reduction Counseling on Blood Glucose and Perceived Stress in Women with Gestational Diabetes. O efeito do aconselhamento para redução do estresse baseado na atenção plena sobre a glicose no sangue e o estresse percebido em mulheres com diabetes gestacional. Rev Bras Ginecol Obstet. 2023;45(9):e517-e523. doi:10.1055/s-0043-1775810
- Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci. 2015;8(3):143-152. doi:10.1016/j.slsci.2015.09.002
- Suffecool K, Rosenn B, Niederkofler EE, et al. Insulin detemir does not cross the human placenta. Diabetes Care. 2015;38(2):e20-e21. doi:10.2337/dc14-2090
About the author
Erin is a registered dietitian and diabetes educator with almost 20 years of experience. She specializes in weight-inclusive diabetes care and prevention, intuitive eating, fitness, and women’s health. She works as a consultant and writer in the health and wellness space. Erin is passionate about empowering people to manage their own health and to have peace with food.