Looking for meal ideas for gestational diabetes? I’ve got you covered! It can be difficult balancing your hunger and blood glucose levels during pregnancy. If you’ve been diagnosed with gestational diabetes, you may be wondering what you can eat. Today, I’m providing some meal ideas for you to manage your glucose levels and achieve a healthy pregnancy.
You’ve done the oral glucose tolerance test and find out that you have gestational diabetes. Now what?
Have you been told to “watch your diet” or “cut carbs”? That can be easier said than done, especially when you are growing a baby and you’re hungry.
So how do you strike a balance between nourishing your body and baby while keeping your blood sugars within target range?
If you’re new here, welcome! I’m Erin, a non-diet registered dietitian and diabetes care and education specialist. Over the last 2 decades, I’ve developed a passion for treating diabetes without restrictive diets.
Sometimes gestational diabetes requires a bit more structure when it comes to meal planning. But that doesn’t mean you can’t enjoy your food.
In this post, I’m giving you meal planning tips, including meal ideas for gestational diabetes. Let’s get started!

Please note: As an Amazon Associate, I earn from qualifying purchases.
What is Gestational Diabetes?
Let’s start with the basics. Gestational diabetes mellitus, or GDM, is a form of diabetes that develops during the later part of pregnancy.
Hormones are being excreted by the placenta throughout the pregnancy which can cause some insulin resistance. To understand gestational diabetes, I’ll explain how insulin works.
When we eat carbohydrates (bread, pasta, rice, fruit, sweets, etc.), they get broken down into glucose (sugar) molecules. Glucose then gets absorbed into the bloodstream.
Our bodies need to get the glucose from the blood into the cells for energy. It is our fuel. To move the glucose, we need insulin.
Insulin is a hormone excreted by our pancreas that enters our bloodstream to transport glucose into the cell for use.

To simplify things even more, think of a car in need of gas. That car is like our cells. We drive the car to a gas station that has the fuel we need. The gas station is our bloodstream.
But for the gas to get from the gas station to the car, we need the pump with the nozzle. If there are no pumps, all of the fuel is stuck at the station, and all of our cars are on empty!
The pump with the nozzle is insulin. It helps get the fuel in the car.
So, the pregnancy hormones cause the insulin to not work as effectively. The glucose, or fuel, gets stuck in the bloodstream. This means the blood glucose or blood sugar levels get too high.
How Do You Manage Gestational Diabetes?

When you’ve been diagnosed with gestational diabetes, you normally start by lowering your blood sugar via diet and exercise.
This is not always the case. Sometimes, if your blood sugar is high enough, you may need to start medication immediately.
The primary medication used to lower blood sugar is insulin. It has been tested to be safe for pregnancy doesn’t cross to the baby.
Insulin is an injectable medication. While you may prefer to take oral medication, they are not often prescribed during pregnancy as they may cross over to the baby.
What if My Blood Sugar Keeps Going Up?

Increasing blood sugar levels are a common occurrence with gestational diabetes.
You finally figure out what food works for you, and then boom. Your blood sugars start to spike.
Here’s why. Your insulin demand goes up greatly in pregnancy and levels off at around 35 weeks.
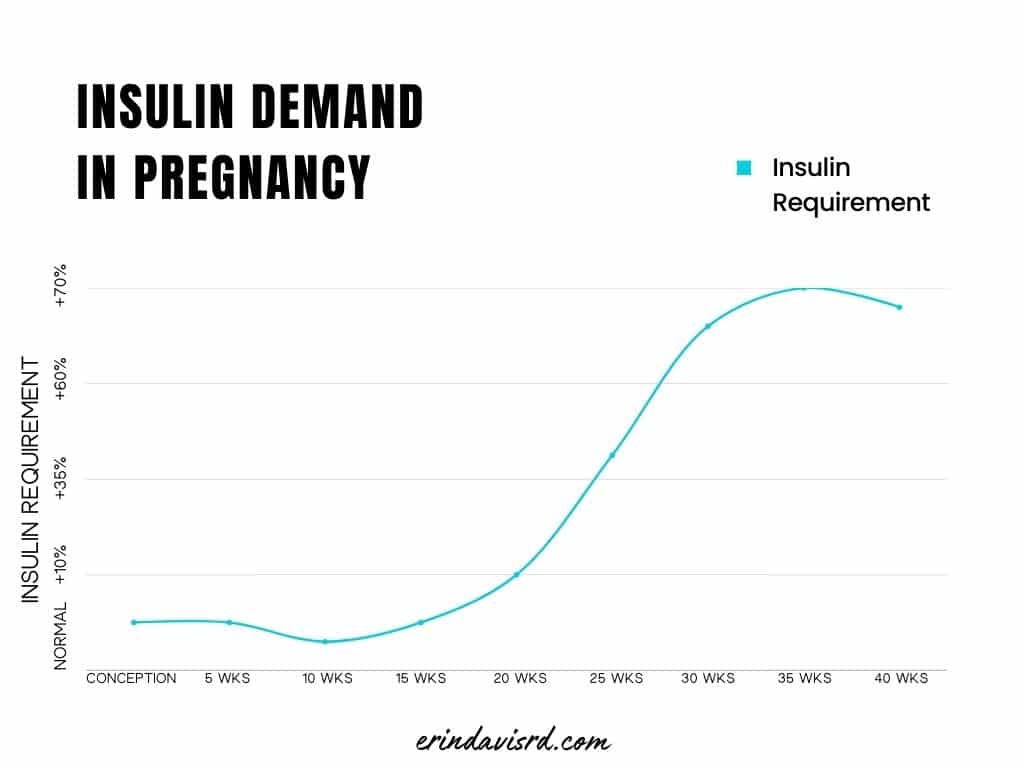
That means what works at 28 weeks may not work at 31 weeks. It’s the nature of gestational diabetes.
The only thing we can do is pivot. Discover patterns in your blood sugars and make tweaks to your meals accordingly.
This is why it’s so important to check your blood sugars at least 3-4 times a day. Here’s a log if you need one.
Additionally, I highly suggest working with a dietitian who specializes in diabetes for this. It doesn’t have to be me. In fact, your OB-GYN probably has a preferred specialist to whom they refer.
If you don’t get your blood sugars down to your target range, you may be at risk for complications during delivery (due to the baby’s larger size and over-production of insulin).
It can be discouraging when your blood sugars go up. However, remind yourself that this will pass.
Having gestational diabetes is not your fault. Your body is producing a crazy amount of hormones and all bodies react differently. Rather than beating yourself up about it, know you aren’t alone and that you can manage it.
Food is a major part of the solution.
What can I eat with Gestational Diabetes?

You can eat anything when you are diagnosed with gestational diabetes.
Yes, that means you can eat pizza. You can eat grapes, apples, bananas, etc.. Yep, you can eat pasta. Plus, you can eat dessert. There’s no forbidden food.
When we eliminate certain food groups from our diet, like fruit or carbs altogether, we’re missing an opportunity for vital nutrients.
Here’s the thing: it’s all about timing and portion.
If your blood sugars run high in the morning, you want to choose a lower-carb breakfast and save your fruit for later in the day.
The same goes if your blood sugars tend to be above target after dinner. Eat the pizza at lunch. And perhaps pair it with a salad or get the thin crust.
Another thing to note is that food order can make a difference. Research has found that eating your protein foods first can help slow digestion and reduce post-meal spikes.
Why Restriction Doesn’t Work
Your diet will need to be personalized to meet your specific needs. But just because it needs to be adjusted, doesn’t mean you can’t eat.
In pregnancy, your body still needs a wide variety of nutrients to support the growth of the baby, delivery, and recovery.
So not only does unnecessary restriction of food groups like carbs reduce your overall nutrient intake, but it can harm your relationship with food.
With gestational diabetes, you are at a higher risk for developing diabetes later in life.
If you are severely restrictive during pregnancy, you will likely go off the rails when baby comes. You can only restrict so long.
Most diets are successful in the short term. As for long-term restrictions, they are not often sustainable.
The goal is to set yourself up for healthy food choices and overall food enjoyment so that you can embrace wellness the rest of your life.
Forbidden foods set you up for food obsession and the binge-restrict cycle. So I strongly encourage you to keep eating your favorite foods, but eat them mindfully.
Eating a variety of foods can ensure you’re getting the nutrients your body needs, and the foods that you enjoy.
Meal Ideas for Gestational Diabetes

Planning meals can be challenging when you are juggling working, parenting, and pregnancy.
You are much less likely to grab fast food or convenience foods if you have a plan in place. Meal ideas for gestational diabetes include:
Breakfast ideas

Breakfast is usually when you have to limit your carbohydrates the most. Our bodies have a difficult time managing large loads of glucose in the morning during pregnancy.
Your dietitian may even have you limit fruit and milk. Although these foods can offer a variety of nutrients, you may need to save them for later in the day.
- Egg on a whole-grain English muffin or a sprouted-grain muffin
- Breakfast burrito with whole grain tortillas (great way to throw in some peppers, onions, spinach, mushrooms, etc.)
- Omelet with cheese, veggies, and avocado
- Instant pot egg bites
- Overnight oats with almond or coconut milk, sweetened with stevia
- Salmon with cream cheese on a whole wheat bagel thin
- Avocado toast
- Plain Greek yogurt with berries
- Chia pudding with chia seeds, almonds, stevia leaf, and berries
- Tofu scramble
Lunch ideas

The middle of the day is often when you can afford to eat more carbohydrates. You’re up, moving, and your insulin works more efficiently.
Here are some ideas for lunch:
- Soup and fruit
- Leftovers (mixed meal of protein/carbohydrate/fat)
- Greens salad with protein (chicken, fish, tofu, eggs, steak, legumes) and olive oil dressing.
- Stir fry with cauliflower rice
- Chopped salad
- Quesadilla with whole wheat tortilla, cheese, meat, peppers and onions
- Tuna or salmon salad on whole wheat crackers
- Sushi with smoked salmon (avoid raw fish)
- Taco salad with seasoned meat, cheese, veggies, and avocado
- Power bowl: on a bed of quinoa, place your favorite protein and sauteed veggies
Dinner ideas

How much carbs you eat for dinner may depend on when you are eating it. Remember, it’s all about the timing and the portions.
If you’re eating a late dinner, you may need to load up on more protein vs. carbohydrates to reduce your morning blood sugar levels.
It should be tailored according to your recent blood sugar levels. Dinner can be anything you’ve made for lunch or these meals:
- Simple protein/carb/veg meal (ie., Fish, sweet potato/quinoa/brown rice, and green vegetable)
- Skillet meal: I like meals that are cooked in one pan so I can eliminate dishes and simplify my meal prep.
- Sheet pan meal: Again, who feels like doing dishes after dinner?
- Slow cooker and Instant Pot meals: Dump-and-go meals are so easy to prepare and my family loves them.
- Egg roll in a bowl
- Stuffed peppers
- Thin crust pizza
- Pasta: you can try low carb or chickpea noodles if you’re struggling with high blood sugars
Reminder: YOU DO NOT NEED SPECIAL FOOD! You can eat what you make for your family. You will just want to make sure you are filling up on protein and vegetables first.
Your post-meal glucose levels will inform you about changes you need to make.
Rather than following a prescriptive and tasteless diet, use your blood sugar data to make small changes to your diet.
This knowledge is extremely valuable when managing your glucose levels throughout your pregnancy.
If you’re struggling, make sure you talk with your dietitian. They can help you make the necessary changes to achieve a healthy pregnancy.
Overwhelmed? I can help. I’ve worked with many women with gestational diabetes to have a healthy pregnancy and delivery.
During an initial assessment, I’ll review your blood sugars and customize your meal plan to your specific nutrient needs. You’ll receive support and feedback on your blood sugar data.
Book a discovery call to meet me here:
Disclaimer: This information is intended as a self-help tool for your own use, at your own risk. My opinions do not reflect the values, thoughts, or opinions of the Academy of Nutrition and Dietetics or other professional health organizations.
About the author
Erin is a registered dietitian and diabetes educator with almost 20 years of experience. She specializes in weight-inclusive diabetes care and prevention, intuitive eating, fitness, and women’s health. She works as a consultant and writer in the health and wellness space. Erin is passionate about empowering people to manage their own health and to have peace with food.


